PATHOGEN INACTIVATION
What is INTERCEPT™ Pathogen Inactivation?
The proactive blood safety solution
The INTERCEPT™ Blood System for Platelets and Plasma is a proactive, holistic solution for hospitals and blood centres, helping to protect patients, improve availability, and deliver significant operational efficiencies.
While blood transfusion infections decline, risks remain
Blood is not tested for many potentially dangerous pathogens and based on the large number of known pathogens and the increase in emerging pathogens, the utility of new tests and donor restrictions will continue to be a challenge. Consideration needs to be given to the cost of developing and implementing new screening assays, the loss of potential donors, and the risk of testing errors. Despite improving the safety of blood components, testing remains a reactive approach to blood safety and relies on the contaminating organisms being identified before sensitive tests can be developed. In contrast, pathogen inactivation (PI) is a proactive strategy designed to inactivate a pathogen and thus prevents transfusion of contaminated blood components.

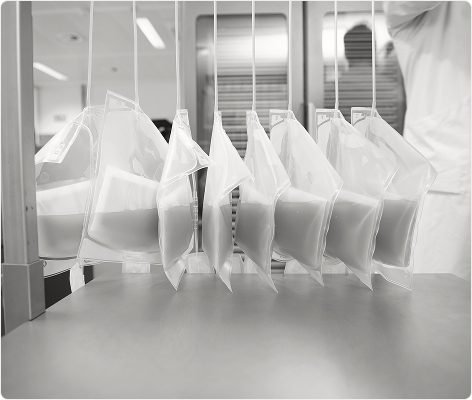
The INTERCEPT™ Blood System
Reliable, robust and the leading PI technology with nearly 20 million units of safer blood components (platelets, plasma) produced to date. It is supported by the broadest level of patient safety data, clinical efficiency, and component quality data than any other pathogen inactivation process.1,2 One solution to address multiple blood safety issues.
 Protects Patients
Protects Patients
Elevated safety and efficacy
The INTERCEPT™ Blood System helps protect patients through proactive, broad-spectrum transfusion transmitted Infections (TTIs) risk reduction by inactivating bacteria, viruses, protozoa and leucocytes. PI technology works via crosslinking nucleic acids (preventing replication and transcription). This addresses both known and unknown risks.

 Improve Availability
Improve Availability
Helps maintain continuity of patient care
The INTERCEPT™ Blood System helps maintain continuity of patient care by helping to ensure platelet and plasma transfusions remain safe and accessible to patients during outbreaks or epidemics.3,4,5 The INTERCEPT™ Blood System also enables to increase shelf life of platelet concentrates, reduce wastage and improve the availability of critical blood components during all times.

 Safeguard Clinical Outcomes
Safeguard Clinical Outcomes
Providing optimal products to patients
The INTERCEPT™ Blood System helps to safeguard clinical outcomes in patients with life threatening diseases or massive bleeding.6,7 Transfusions of platelets and plasma are an integral part of sometimes very expensive treatment schemes. Pathogen contamination of blood components poses an important risk to the success of those therapies, potentially causing undesirable adverse events or secondary infections in severely ill patients.

 Provide Operational Benefits
Provide Operational Benefits
Realise significant operational efficiencies
The INTERCEPT™ Blood System allows significant operational efficiencies at many steps of the transfusion chain. Simplification in donor selection and donor testing, enabling of more cost-effective/optimised collection and production methods and reduced waste of critical blood components, which translates into cost savings or incremental revenue that could offset partially or completely the investment cost for INTERCEPT™ Blood System. The INTERCEPT™ Blood System treatment of plasma and platelets can occur on the same Illuminator platform for optimal efficiency.
You may also be interested in
- Platelet Additive Solutions and Pathogen Reduction Impact on Transfusion Safety, Patient Management and Platelet Supply; Georges Andreu; Transfusion Medicine Reviews 39 (2025) 150875
- Therapeutic efficacy and safety of pathogen-reduced platelet components: Results of a meta-analysis of randomized controlled trials; J Cid et al; Vox Sang. 2024 Mar;119(3):203-211. doi: 10.1111/vox.13573. Epub 2024 Jan 5.
- Inactivation of Zika virus in plasma with amotosalen and ultraviolet A illumination; Maite Aubry et al; Transfusion 2016 Jan;56(1):33-40.doi: 10.1111/trf.13271. Epub 2015 Aug 18.
- Emergency response of four transfusion centers during the last Chikungunya outbreak in Italy; Luca Pierelli et al; Transfusion 2018;58; 3027-3030
- Mitigating the risk of transfusion-transmitted infections with vector-borne agents solely by means of pathogen reduction; Susan I. Stramer et al; Transfusion. 2022 Jul;62(7):1388-1398. doi: 10.1111/trf.16950. Epub 2022 Jun 21
- Nussbaumer W et al., 2017. Patient outcomes and amotosalen/UVA-treated platelet utilization in massively transfused patients. Vox Sang 112: 249-256
- Cid J et al., 2024. Therapeutic efficacy and safety of pathogen-reduced platelet components: Results of a meta-analysis of randomized controlled trials. Vox Sang 119: 203-211
There is no pathogen inactivation process that has been shown to eliminate all pathogens. Certain non-enveloped viruses (e.g., HAV, HEV, B19, and poliovirus) and Bacillus cereus spores have demonstrated resistance to the INTERCEPT™ process. For a full list of warnings, precautions for use and pathogens inactivated, please refer to the Technical Data Sheet and Instructions for Use found in the resource section of this website.


